|
|
Quiz (Ch. 37) Quiz (Ch. 38) |
Selected bacterial diseases |
|
|
|
Lecture Index | ||
|
|
Course Resources page |
Last revised: Monday, April 24, 2000
Ch. 37, 38 in Prescott et al, Microbiology, 4th Ed.Note: These notes are provided as a guide to topics the instructor hopes to cover during lecture. Actual coverage will always differ somewhat from what is printed here. These notes are not a substitute for the actual lecture!Copyright 2000. Thomas M. Terry
Bacterial Disease Case Study: Staph infections
- Staphylococcus aureus is so common that it is hard to appreciate the full range of its virulence.
- S. aureus is an opportunist, a common member of normal flora that rarely afflicts healthy individuals, but can seize on sudden opportunity (such as a break in the skin, a burn, or a superabsorbent tampon) to turn vicious, activating an extraordinary range of virulence factors. Over all of human history, S. aureus may be responsible for more collective suffering and pain than any other single bacterium!
- S. aureus infections are especially common in hospitals. About 1/3 of strains isolated from hospitalized infections are now resistant to all antibiotics except vancomycin, and resistant strains to that drug are beginning to show up!
- Diseases caused by S. aureus include:
- boils and abcesses
- cellulitis
- furuncles and carbuncles
- impetigo and "scaled skin" syndrome
- pneumonia, endocarditis, and septicemia
- toxic shock syndrome:
- many strains of Staph. aureus release "superantigens", act asactivators of T-cells.
- Normally, a foreign antigen might cause 0.001% of T-cell population to divide; superantigen can cause 2-20% to divide.
- Result = upset delicate balance that normally keeps T-cell response very local and specific; instead, many T-cells are killed, much energy is wasted in ways that don't harm pathogen. Responsible for "Toxic shock syndrome".
- S. aureus carries a number of virulence factors, including:
- an exotoxin that causes skin layers to separate and slough off (scalded skin syndrome)
- an enterotoxin that causes vomiting and diarrhea
- an exotoxin that causes toxic shock syndrome, leading to death
- the enzyme coagulase, that coagulates blood and prevents phagocytes from reaching the site of infection
- enzymes called leukocidins that kill phagocytes, resulting in pus
- and many more .....
- Recently, scientists have begun to understand how virulence factors in S. aureus are regulated. RAP (RNAIII activating protein) controls production of toxins and other virulence proteins. Naomi Balaban discovered RAP a few years ago, and suggested that this protein shifts S. aureus from early stage of infection (attachment) into its later stage of infection (virulence), turning on toxins and other enzymes.
- If animals could be immunized against RAP, might be possible to "short-circuit" the expression of Staph virulence factors. A report in the journal Science, 280:438-440 (1998) published April 17, 1998 suggests this possibility.
Entry of Pathogens into hosts
- Diseases often categorized based on "Portal of Entry" into host.
- Entry via respiratory tract =Airborne diseases
- Air inside building contains 500-1000 microbes/cubic meter of air, and humans breathe 6 liters/min at rest. So up to 10,000 microbes per day enter lungs.
- Most are expelled by "mucociliary elevator" = combined action of cilia beating upwards in bronchioles and mucus secretions that trap airborne particles. Result is that alveoli (air sacs in lung) get few microbes. Those that do reach alveoli are quickly eaten by macrophages.
- Exceptions: Mycobacterium tuberculosis, gets into lungs, survives inside macrophages (blocks fusion with lysosomes). Result: body responds by trying to wall off infected macrophages = tubercules, accumulate in lung tissue and can show up on X-rays. Diseased hosts have difficulty breathing, cough frequently.
- Examples of airborne pathogens
- Diphtheria. Caused by Corynebacterium diphtheriae. See lecture notes from Univ. of Wisconsin.
- Bacterial meningitis. Caused by a variety of different bacteria (and viruses). See CDC fact sheet.
- Pertussis. See "Bordetella pertussis and Whooping Cough" lecture notes from Univ. of Wisconsin.
- Streptococcal diseases: cellulitis & impetigo, invasive strep A infections, rheumatic fever, strep throat, streptococcal pneumonia. See CDC fact sheet on group A streptococcal infections.

Hemolysis produced by colonies of Streptococcus pyogenes
- Tuberculosis. See CDC fact sheet.
- Arthropod-Borne diseases
- Many pathogens depend on insect or other arthropod bites to break skin.
- Examples of airborne pathogens
- Lyme disease . Caused by Borrelia burgdorferi. See CDC fact sheet.
- Plague . Caused by Yersinia pestis. See CDC fact sheet.
- Epidemic typhus . Caused by Rickettsia, obligate intracellular bacteria.
- Direct Contact diseases
- Skin contact can transmit pathogens from host to host. Can occur between animals and humans, or from casual or intimate (venereal) human-human contact.
- Examples of airborne pathogens
- Anthrax . from Bacillus anthracis found on infected domestic animals. See CDC fact sheet.
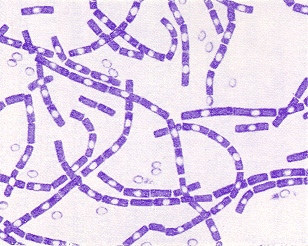
Gram stain of Bacillus anthracis, showing endospores.
- Staphylococcal infections. Caused by Staphylococcus aureus. See CDC fact sheet on vancomycin-resistant staph; CDC fact sheet on toxic shock syndrome.
- Gonorrhea . Caused byNeisseria gonorrhoeae. ---> gonorrhea, infects urinary tract in men, painful urination and pus-like discharge from penis. Gonococcus strains have pili that attach to epithelium (mutants lacking pili are not infectious). Bacteria are engulfed by cells, grow intracellularly, protected from washout. Males rarely get bladder infections except when using catheters or when not urinating frequently. Urethra is 20 cm long (in flaccid state).
View gonococci in epithelial tissue.
See CDC fact sheet.- Nongonoccocal urethritis. Caused by strains of Chlamydia trachomatis, also called "chlamydiasis." The most common sexually transmitted disease (STD) in the U.S., with around 4,000,000 cases/year, mostly in the 15-25 year age group. See CDC fact sheet.
- Trachoma . Another chlamydial disease, caused by Chlamydia trachomatis.
- Entry via GI tract = food-borne and waterborne diseases
Stomach acids and bile salts in intestines (detergent) kill most microbes. Dose of microbes critical to establishment of disease. May need to ingest as many as 108 bacteria to get enough survivors into intestine to cause disease.
- Stomach was long thought to be too acidic for bacterial survival. Recently, Helicobacter pylori found to be able to grow in stomach and to cause ulcers.
- Some Gram-negatives survive (includes group known as "enterics": Shigella, Salmonella, etc.), certain strains can cause disease.
- Lining of intestinal tract is shed every 3 days, so bacteria must continue to grow and reproduce or they will lose their "place".
- Some intestinal pathogens good at binding to epithelium: ex. Vibrio cholera (causes cholera), certain strains of E. coli, Shigella, Salmonella, etc.
Take a Self-Quiz on Ch. 37 material
Take a Self-Quiz on Ch. 38 material
Return to Lecture Index
Return to MCB 229 Course Resources page